Indications and Usage
Thyrogen® (thyrotropin alfa), for intramuscular use
INDICATIONS AND USAGE
Thyrogen® (thyrotropin alfa) is a thyroid stimulating hormone indicated for:
Adjunctive Diagnostic Tool for Well-Differentiated Thyroid Cancer: Use as an adjunctive diagnostic tool for serum thyroglobulin (Tg) testing with or without radioiodine imaging in the follow-up of patients with well-differentiated thyroid cancer who have previously undergone thyroidectomy.
Limitations of Use:
- Thyrogen-stimulated Tg levels are generally lower than, and do not correlate with Tg levels after thyroid hormone withdrawal.
- Even when Thyrogen-Tg testing is performed in combination with radioiodine imaging, there remains a risk of missing a diagnosis of thyroid cancer or underestimating the extent of the disease.
- Anti-Tg Antibodies may confound the Tg assay and render Tg levels uninterpretable.
Adjunct for Thyroid Remnant Ablation in Well-Differentiated Thyroid Cancer: Use as an adjunctive treatment for radioiodine ablation of thyroid tissue remnants in patients who have undergone a near-total or total thyroidectomy for well-differentiated thyroid cancer and who do not have evidence of distant metastatic thyroid cancer.
Limitations of Use:
- The effect of Thyrogen on thyroid cancer recurrence greater than 5 years post-remnant ablation has not been evaluated.
The Uses of Thyrogen

Thyrogen allows your patients to stay on their hormone replacement medication during ablation
Learn how thyroid hormone withdrawal can cause acute hypothyroidism.

Thyrogen allows your patient to stay on their hormone replacement therapy during their diagnostic testing
Understand why your doctor has recommended Thyrogen and how it may help.
Learn more about the use of Thyrogen in risk stratification and selection of patients for radioactive iodine ablation
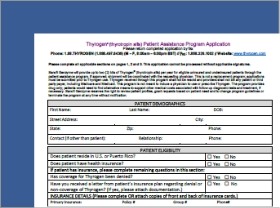
Sanofi provides various services to help patients access Thyrogen® (thyrotropin alfa).
Choose how to get Thyrogen (thyrotropin alfa) for your patients
Not sure which one to choose? Contact ThyrogenONE for assistance

Option 1: Sign up or log into the ThyrogenONE portal
The ThyrogenONE portal provides your office online access to help you and your patients :
- Submit and track benefit verifications
- Coordinate orders
- Generate automatic alerts

Option 2: Call ThyrogenONE at 1-88-THYROGEN (1-888-497-6436) (
Dedicated ThyrogenONE Case Managers can assist you and your patients with the following.
- Benefits Verification
- Information on Ordering
- Information on specialty pharmacy fulfillment
The Impact Of Thyrogen: Watch Videos on Patient and Doctor Perspectives
- The effect of Thyrogen on long term thyroid cancer outcomes has not been determined.
- When Thyrogen is used to help detect thyroid cancer, there is still a chance all or parts of the cancer could be missed.
- In a study of people being prepared for treatment with a form of iodine after thyroid surgery, results were similar between those who received Thyrogen and those who stopped taking their thyroid hormone for up to 5 years after treatment. Researchers do not know if results would be similar over a longer period of time.
- There have been reports of events that led to death in patients who not had surgery to have their thyroid gland removed, and in patients with thyroid cancer cells that have spread to other parts of the body.
- Patients over 65 years old with large amounts of leftover thyroid tissue after surgery, or with a history of heart disease, should discuss with their physicians the risks and benefits of Thyrogen.
- Thyrogen can be administered in the hospital for patients at risk for complications from Thyrogen administration.
- Since Thyrogen was first approved for use, there have been reports of central nervous system problems such as stroke in young women who have a higher chance of having a stroke, and weakness on one side of the body. The relationship between Thyrogen administration and stroke is unknown. Patients should remain hydrated prior to treatment with Thyrogen.
- Leftover thyroid tissue after surgery and cancer cells that have spread to other parts of the body can quickly grow and become painful after Thyrogen administration. Patients with cancer cells near their windpipe, in their central nervous system, or in their lungs may need treatment with a glucocorticoid (a medication to help prevent an increase in the size of the cancer cells before using Thyrogen.)
- If THYROGEN is administered with radioiodine (RAI), the serious side effects for RAI apply to this combination regimen. Please consult with your doctor for a list of contraindications for radioiodine.
- The effect of Thyrogen on long term thyroid cancer outcomes has not been determined.
- When Thyrogen is used to help detect thyroid cancer, there is still a chance all or parts of the cancer could be missed.
- In a study of people being prepared for treatment with a form of iodine after thyroid surgery, results were similar between those who received Thyrogen and those who stopped taking their thyroid hormone for up to 5 years after treatment. Researchers do not know if results would be similar over a longer period of time.
Please note:
Patient – Red Text
Physician – Green Text
Safety – Black Text
I. Opening Safety Information
INDICATIONS AND USAGE with voiceover
Thyrogen (thyrotropin alfa) is used to help identify thyroid disease by testing the blood for a hormone called thyroglobulin in the follow up of patients with a certain type of thyroid cancer known as well differentiated thyroid cancer. It is used with or without a radiology test using a form of iodine.
Limitations of Use:
Thyrogen is also used to help patients prepare for treatment with a form of iodine, called radioiodine, to remove leftover thyroid tissue in patients who have had surgery to take out the entire thyroid gland for patients with well differentiated thyroid cancer who do not have signs of thyroid cancer which has spread to other parts of the body.
Limitations of Use:
II. Video Introduction
My name is Amy. I live in Salem, New Hampshire.
I recently got married last year and I'm a trainer for a biotech company in Cambridge, Massachusetts.
So I found out that I had thyroid cancer. I was told it's a good cancer to have. You know, you're going to have your thyroid removed. You're going to be on medication for the rest of your life. Well, I knew I had to have my thyroid removed. I mean that is standard of care. It is a pretty routine procedure.
I met Amy because she was being prepared for her first one year follow-up stimulated whole body scan and she was not able to get Thyrogen from the academic center that she was being seen at and wanted a second opinion about how to manage her thyroid cancer. She was very educated and she knew that she could have used the Thyrogen for her initial ablation. Her physician that was managing her disease did not prefer to use it so she actually went through the hypothyroidism.
III. 1st Ablation/Hypothyroidism
I was preparing for the ablation. So now they have to give me an artificial medication. Just act like I have a thyroid. Synthroid is because I don't have a thyroid. They told me I had to go through withdrawal so I said, okay, tell me a little bit about this. What's going to happen when I go hypothyroid? You'll be uncomfortable. You can still work, and you have to go on this low iodine diet. I said, okay.
So I started going to work, and after about maybe a week, I went on medical leave. I couldn't focus on anything. I typed emails. There were some mistakes on every page. I felt like I was walking in peanut butter. I think I gained 22 pounds, eating nothing—really, eating next to nothing. I used to describe it as like being, now that I have a 13-year-old stepdaughter, being hyper-emotional. I mean once I said it's like having an out of body experience and watching yourself do things, and you can't control it or being hyper- emotional because you would start to cry. But you know that it's happening, and you can't control yourself. You also feel like you're constantly in a brain fog and everything's an effort. Like there's just such a disconnect between what you're doing.
Remember what you do, you stop the medication for three to four weeks. You do the therapy and then when you restart the thyroid hormone, it takes another four to eight weeks to recover so you end up being hypothyroid for a total of three months.
IV. 2nd Ablation/Thyrogen
So when I was talking to other people, very knowledgeable about thyroid cancer or what I was going through, they said, I think you have an obligation to talk to somebody else. At least go get a second opinion. So that's when I was given the name of Dr. Lee, and I reached out to Dr. Lee.
And I went in there explaining what I had been through and when she said what she thought, you know, what she wanted to do, which was a second ablation. I said, first of all, I've been through hypothyroidism. I really don't want to go through that again. And I'm very familiar with thyrogen. And she said, well, of course, I would use thyrogen.
She really did not want to become hypothyroid again; and actually, came to me requesting whether a recombinant human TSH or Thyrogen would be useful in her particular case? I said yes. Her post-therapy scan showed iodine uptake into local nodes. But after that, her thyroglobulin in her blood did not fall. That told me that she had significant residual disease. And her original institution was going to make her hypothyroid again to do a whole body scan for localization. And she came to me saying, "Is this the best way to manage that?"
So, for Thyrogen, I had to come into the office, I think, a total of three days. I had to come in and get the injection and had to come in to the office for follow-up.
So now experiencing thyrogen, it's a little injection in your butt. So maybe people don’t like that. I didn't have to miss work, I felt no different.
It was simple. I would say, if there was an option provided, patients should definitely look into Thyrogen.
V. Scrolling ISI/with Professional Voiceover
IMPORTANT SAFETY INFORMATION
Patients should not use Thyrogen with radioiodine if they have a contraindication to the use of radioiodine. Please consult with your doctor for a list of contraindications for radioiodine.
Thyrogen can cause serious side effects, including:
Thyrogen-Induced Hyperthyroidism:
Stroke:
Sudden Rapid Tumor Enlargement:
Risks Associated with Radioiodine Treatment:
ADVERSE REACTIONS
In clinical studies, the most common side effects reported were nausea and headache.
USE IN SPECIFIC PATIENT POPULATIONS
Pregnant patients: Notify your healthcare provider immediately in the event of a pregnancy. If Thyrogen is administered with radioiodine, the combination regimen should not be used in pregnant women. Thyrogen should be given to a pregnant woman only if the doctor thinks there is a clear need for it.
Breastfeeding patients:If Thyrogen is administered with radioiodine, the combination regimen should not be used in breastfeeding women. It is not known whether Thyrogen can appear in human milk. Breastfeeding women should discuss the benefits and risks of Thyrogen with their physician.
Children: Safety and effectiveness in young patients (under the age of 18) have not been established.
Elderly: Studies do not show a difference in the safety and effectiveness of Thyrogen between adult patients less than 65 years and those over 65 years of age.
Patients with kidney disease: Thyrogen exits the body much slower in dialysis patients and can lead to longer high TSH levels.
Indications and Usage:
Thyrogen (thyrotropin alfa) is used to help identify thyroid disease by testing the blood for a hormone called thyroglobulin in the follow up of patients with a certain type of thyroid cancer known as well differentiated thyroid cancer. It is used with or without a radiology test using a form of iodine.
Limitations of Use:
Thyrogen is also used to help patients prepare for treatment with a form of iodine, called radioiodine, to remove leftover thyroid tissue in patients who have had surgery to take out the entire thyroid gland for patients with well differentiated thyroid cancer who do not have signs of thyroid cancer which has spread to other parts of the body.
Limitations of Use:
This patient story reflects the real-life experience of a person diagnosed with thyroid cancer who has been prescribed Thyrogen. However, individual experiences may vary. Patient stories are not necessarily representative of what another person using Thyrogen may experience. Sanofi Genzyme does not provide medical advice, diagnosis, or treatment. The health information contained herein is provided for general educational purposes only. Your healthcare professional is the best source of information regarding your health. Please consult your healthcare professional if you have any questions about your health or treatment.
Please visit www.thyrogen.com for full prescribing information
MAT-US-2006958
April 2020
© 2020 Genzyme Corporation. All rights reserved.
Thyrogen, Sanofi and Genzyme are registered in the U.S. Patent and Trademark Office
Impact of Thyrogen versus Thyroid Hormone Withdrawal (THW) – A Patient’s Story
Watch Amy, a thyroid cancer patient, explain how Thyrogen (thyrotropin alfa) helps alleviate some of the signs and symptoms of hypothyroidism caused by thyroid hormone withdrawal (THW).
- The effect of Thyrogen on long term thyroid cancer outcomes has not been determined.
- When Thyrogen is used to help detect thyroid cancer, there is still a chance all or parts of the cancer could be missed.
- In a study of people being prepared for treatment with a form of iodine after thyroid surgery, results were similar between those who received Thyrogen and those who stopped taking their thyroid hormone for up to 5 years after treatment. Researchers do not know if results would be similar over a longer period of time.
- 0.9 mg IM Thyrogen dose q24 hours for 2 doses (days 1 and 2) Day 3
- If performing a whole-body scan (WBS), 4 mCi of 131I is given on day 3 (24 hours after the last Thyrogen injection)
- Serum Tg is measured on day 5 (72 hours after the last Thyrogen injection) when average Tg levels peak
- WBS is performed on day 5 (72 hours after last Thyrogen injection
- 0.9 mg IM Thyrogen dose q24 hours for 2 doses. Days 1 and 2 Day 3
- For remnant ablation with Thyrogen 131I is given on day 3 24 hours after the last Thyrogen injection. The dose of 131I is selected at the discretion of the physician.
- A post ablation scan should be performed 3-7 days after the administration of 131I
- There have been reports of events that led to death in patients who not had surgery to have their thyroid gland removed, and in patients with thyroid cancer cells that have spread to other parts of the body.
- Patients over 65 years old with large amounts of leftover thyroid tissue after surgery, or with a history of heart disease, should discuss with their physicians the risks and benefits of Thyrogen.
- Thyrogen can be administered in the hospital for patients at risk for complications from Thyrogen administration.
- Since Thyrogen was first approved for use, there have been reports of central nervous system problems such as stroke in young women who have a higher chance of having a stroke, and weakness on one side of the body. The relationship between Thyrogen administration and stroke is unknown. Patients should remain hydrated prior to treatment with Thyrogen.
- Leftover thyroid tissue after surgery and cancer cells that have spread to other parts of the body can quickly grow and become painful after Thyrogen administration. Patients with cancer cells near their windpipe, in their central nervous system, or in their lungs may need treatment with a glucocorticoid (a medication to help prevent an increase in the size of the cancer cells before using Thyrogen.)
- If THYROGEN is administered with radioiodine (RAI), the serious side effects for RAI apply to this combination regimen. Please consult with your doctor for a list of contraindications for radioiodine.
- The effect of Thyrogen on long term thyroid cancer outcomes has not been determined.
- When Thyrogen is used to help detect thyroid cancer, there is still a chance all or parts of the cancer could be missed.
INDICATIONS AND USAGE with voiceover
Thyrogen (thyrotropin alfa) is used to help identify thyroid disease by testing the blood for a hormone called thyroglobulin in the follow up of patients with a certain type of thyroid cancer known as well differentiated thyroid cancer. It is used with or without a radiology test using a form of iodine.
Limitations of Use:
Thyrogen is also used to help patients prepare for treatment with a form of iodine, called radioiodine, to remove leftover thyroid tissue in patients who have had surgery to take out the entire thyroid gland for patients with well differentiated thyroid cancer who do not have signs of thyroid cancer which has spread to other parts of the body.
Limitations of Use:
I. Introduction
My name is Stephanie Lee, I'm a professor of medicine at Boston Medical Center. My interest in primarily in thyroid disease, both thyroid nodules and thyroid cancer. I just realized I had my 30th anniversary after finishing my fellowship this year. I see a lot of patients per year, primarily all of the patients that I see are thyroid-related patients. I probably have about 700 or 800 thyroid cancer patients,
I will tell people that the thyroid hormone is your everyday cancer therapy because if the thyroid hormone is not taken and you're hypothyroid, endogenous TSH goes up. So I tell patients as the thyroid stimulating hormone, there's also thyroid cancer stimulating hormone. So our goal is to keep that as low as possible. And you can only achieve that if you take your medication regularly. So I think those are some of the things that are lessons to tell patients and not to scare the young patients quite so much.
II. Patient Selection - Thyrogen Treatment
So the question is when do we use Thyrogen for radioactive iodine treatment and what patient might we consider actually taking them off thyroid hormone and making them hypothyroid? So the usual patient who gets therapy now is being stimulated using Thyrogen. The reason is there's been a number of hallmark papers published in the last five years looking at the equivalents of radioactive iodine where there's given 30 or 100 millicuries hypothyroid or with Thyrogen. And all four groups were actually identical in response. So because of that, in patients who have the usual thyroid cancer we will do the treatment with recombinant human TSH.
III. Understanding Thyrogen
Thyrogen actually is identical to a hormone made in your pituitary. And the pituitary and the thyroid work a little bit like a thermostat. So when the pituitary realizes there's not enough thyroid hormone, like the thyroid hormone levels are too low, it sends a pulse out to the thyroid and tells the thyroid to make more hormones. So that pulse is TSH, a thyroid stimulating hormone.
If, for some reason, the thyroid is making too much hormone, it feeds back to the brain. And the brain says, oh, I don’t need to make any more thyroid hormone. So the TSH goes down, and then it turns off the thyroid.
We can exploit that concept of the TSH stimulating the thyroid to take up iodine and to make thyroglobulin, which is part of the thyroid hormone molecule, for our use in thyroid cancer. So we use that hormone to stimulate the thyroid for two reasons. One is, if we just want to know if it's a residual tumor, you can do the two injections and just measure a blood test five days later for thyroglobulin. And if the thyroglobulin is less than 2.0 we consider that to be a negative test saying that there's unlikely to be significant residual tumor there. On the other hand, if we want to know where the thyroid cancer is, generally, in the usual, typical pathway carcinoma and follicular carcinoma, if we give a dose of radioactive iodine stimulated with the Thyrogen, it will go to the tumor cells, and they will take up the iodine, and then we can see it on a scan.
So those are the two diagnostic things we do.
IV. Thyrogen Treatment Experience
In fact, have to have someone who's been around for a while because we've done just the Thyrogen for so long that it's unusual to see someone who's been withdrawn. But I think it also depends of where you live in the country. So I will meet a patient who's had hypothyroid withdrawal versus Thyrogen.
So how do I tell my patients to prepare for the radioactive iodine therapy? So in the past, when we made them hypothyroid, I'd write them letters. I used to have an entire paragraph saying if you operate heavy equipment, if you feel like you're too drowsy, you shouldn’t be driving a car, you should not be doing anything that requires balance. And now, with the Thyrogen use, I no longer put that in my letters. I've taken that out or added in for those few patients who will get hypothyroid.
The rest of the preparation is really preparing them to reduce their iodine load, to come in for the injections and then the therapy and then the complications after therapy.
V. Dosing
There are two protocols to follow regarding Thyrogen injection. Diagnostic and ablation. The following protocol is recommended for diagnostic testing with Thyrogen. Day 1 and 2.
Day 5
- WBS should be acquired for at least 30 minutes and/or should contain >140,000 counts
The following protocol is recommended for ablation with Thyrogen.
Day 1 and 2
Days 6-10
Pretreatment with glucocorticoids should be considered for patients in whom tumor expansion may compromise vital anatomic structures.
VI. Scrolling ISI/with Professional Voiceover
IMPORTANT SAFETY INFORMATION
Patients should not use Thyrogen with radioiodine if they have a contraindication to the use of radioiodine. Please consult with your doctor for a list of contraindications for radioiodine.
Thyrogen can cause serious side effects, including:
Thyrogen-Induced Hyperthyroidism:
Stroke:
Sudden Rapid Tumor Enlargement:
Risks Associated with Radioiodine Treatment:
ADVERSE REACTIONS
In clinical studies, the most common side effects reported were nausea and headache.
USE IN SPECIFIC PATIENT POPULATIONS
Pregnant patients: Notify your healthcare provider immediately in the event of a pregnancy. If Thyrogen is administered with radioiodine, the combination regimen should not be used in pregnant women. Thyrogen should be given to a pregnant woman only if the doctor thinks there is a clear need for it.
Breastfeeding patients: If Thyrogen is administered with radioiodine, the combination regimen should not be used in breastfeeding women. It is not known whether Thyrogen can appear in human milk. Breastfeeding women should discuss the benefits and risks of Thyrogen with their physician.
Children: Safety and effectiveness in young patients (under the age of 18) have not been established.
Elderly: Studies do not show a difference in the safety and effectiveness of Thyrogen between adult patients less than 65 years and those over 65 years of age.
Patients with kidney disease: Thyrogen exits the body much slower in dialysis patients and can lead to longer high TSH levels.
Indications and Usage: Thyrogen (thyrotropin alfa) is used to help identify thyroid disease by testing the blood for a hormone called thyroglobulin in the follow up of patients with a certain type of thyroid cancer known as well differentiated thyroid cancer. It is used with or without a radiology test using a form of iodine.
Limitations of Use:
Thyrogen is also used to help patients prepare for treatment with a form of iodine, called radioiodine, to remove leftover thyroid tissue in patients who have had surgery to take out the entire thyroid gland for patients with well differentiated thyroid cancer who do not have signs of thyroid cancer which has spread to other parts of the body.
Limitations of Use:
In a study of people being prepared for treatment with a form of iodine after thyroid surgery, results were similar between those who received Thyrogen and those who stopped taking their thyroid hormone for up to 5 years after treatment. Researchers do not know if results would be similar over a longer period of time.
Please visit www.thyrogen.com for full prescribing information
MAT-US-2006958
April 2020
© 2020 Genzyme Corporation. All rights reserved. Thyrogen, Sanofi and Genzyme are registered in the U.S. Patent and Trademark Office
The Benefits of Thyrogen versus Thyroid Hormone Withdrawal (THW) – A Doctor’s Perspective
Watch Dr. Stephanie Lee, MD, PhD, Associate Chief, Section of Endocrinology, Nutrition and Diabetes of Boston Medical Center, share her perspective on how Thyrogen (thyrotropin alfa) helps thyroid cancer patients in preparation for radioactive iodine (RAI) ablation treatment and monitoring for progression.
Important Safety Information and Indications
Important Safety Information and Indications
IMPORTANT SAFETY INFORMATION
CONTRAINDICATIONS
If Thyrogen is administered with radioiodine, the contraindications to radioiodine also apply to this combination regimen. Refer to the radioiodine prescribing information for a list of contraindications for radioiodine.
WARNINGS AND PRECAUTIONS
Thyrogen-Induced Hyperthyroidism:
- There have been reports of death in non-thyroidectomized patients and in patients with distant metastatic thyroid cancer in which events leading to death occurred within 24 hours after administration of Thyrogen. Caution should be exercised in patients who have substantial thyroid tissue still in situ or functional thyroid cancer metastases, specifically in the elderly and those with a known history of heart disease.
- Hospitalization for administration of Thyrogen and post-administration observation in patients at risk should be considered.
Stroke:
- There are post marketing reports of stroke in young women with risk factors for stroke, and neurological findings suggestive of stroke (e.g., unilateral weakness) occurring within 72 hours of Thyrogen administration in patients without known central nervous system metastases. The relationship between Thyrogen administration and stroke is unknown. Patients should be well-hydrated prior to treatment with Thyrogen.
Sudden Rapid Tumor Enlargement:
- Sudden, rapid and painful enlargement of residual thyroid tissue or distant metastases can occur following treatment with Thyrogen. Pretreatment with glucocorticoids should be considered for patients in whom tumor expansion may compromise vital anatomic structures.
Risks Associated with Radioiodine Treatment:
- If Thyrogen is administered with radioiodine (RAI), the warnings and precautions for RAI apply to this combination regimen. Refer to the RAI prescribing information for a full list of the warnings and precautions for RAI.
ADVERSE REACTIONS
The most common adverse reactions reported in clinical trials were nausea and headache.
USE IN SPECIFIC POPULATIONS
Pregnancy:
- If Thyrogen is administered with radioiodine, the combination regimen is contraindicated in pregnant women.
- Available data with Thyrogen use in pregnant women are insufficient to evaluate for a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes.
Lactation:
- The concomitant use of Thyrogen and radioiodine (RAI) is contraindicated in lactating women. If Thyrogen is administered with RAI for diagnostic use, discontinue breastfeeding after RAI administration because of the potential for serious adverse reactions from RAI in the breastfed infant.
- If Thyrogen is not administered with RAI, the developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Thyrogen and any potential adverse effects on the breastfed child. There are no available data on the presence of thyrotropin alfa in human milk, the effects on the breastfed infant, or the effects on milk production.
Pediatric Use: Safety and effectiveness in pediatric patients have not been established.
Geriatric Use: Results from controlled trials do not indicate a difference in the safety and efficacy of Thyrogen between adult patients less than 65 years and those over 65 years of age.
Renal Impairment: Elimination of Thyrogen is significantly slower in dialysis-dependent end stage renal disease patients, resulting in prolonged elevation of TSH levels.
INDICATIONS AND USAGE
Thyrogen® (thyrotropin alfa) is a thyroid stimulating hormone indicated for:
Adjunctive Diagnostic Tool for Well-Differentiated Thyroid Cancer: Use as an adjunctive diagnostic tool for serum thyroglobulin (Tg) testing with or without radioiodine imaging in the follow-up of patients with well-differentiated thyroid cancer who have previously undergone thyroidectomy.
Limitations of Use:
- Thyrogen-stimulated Tg levels are generally lower than, and do not correlate with Tg levels after thyroid hormone withdrawal.
- Even when Thyrogen-Tg testing is performed in combination with radioiodine imaging, there remains a risk of missing a diagnosis of thyroid cancer or underestimating the extent of the disease.
- Anti-Tg Antibodies may confound the Tg assay and render Tg levels uninterpretable.
Adjunct for Thyroid Remnant Ablation in Well-Differentiated Thyroid Cancer: Use as an adjunctive treatment for radioiodine ablation of thyroid tissue remnants in patients who have undergone a near-total or total thyroidectomy for well-differentiated thyroid cancer and who do not have evidence of distant metastatic thyroid cancer.
Limitations of Use:
- The effect of Thyrogen on thyroid cancer recurrence greater than 5 years post-remnant ablation has not been evaluated.
Click here for full Prescribing Information
Important Safety Information and Indications
IMPORTANT SAFETY INFORMATION
CONTRAINDICATIONS
If Thyrogen is administered with radioiodine, the contraindications to radioiodine also apply to this combination regimen. Refer to the radioiodine prescribing information for a list of contraindications for radioiodine.
WARNINGS AND PRECAUTIONS
Thyrogen-Induced Hyperthyroidism:
- There have been reports of death in non-thyroidectomized patients and in patients with distant metastatic thyroid cancer in which events leading to death occurred within 24 hours after administration of Thyrogen. Caution should be exercised in patients who have substantial thyroid tissue still in situ or functional thyroid cancer metastases, specifically in the elderly and those with a known history of heart disease.
- Hospitalization for administration of Thyrogen and post-administration observation in patients at risk should be considered.
Stroke:
- There are post marketing reports of stroke in young women with risk factors for stroke, and neurological findings suggestive of stroke (e.g., unilateral weakness) occurring within 72 hours of Thyrogen administration in patients without known central nervous system metastases. The relationship between Thyrogen administration and stroke is unknown. Patients should be well-hydrated prior to treatment with Thyrogen.
Sudden Rapid Tumor Enlargement:
- Sudden, rapid and painful enlargement of residual thyroid tissue or distant metastases can occur following treatment with Thyrogen. Pretreatment with glucocorticoids should be considered for patients in whom tumor expansion may compromise vital anatomic structures.
Risks Associated with Radioiodine Treatment:
- If Thyrogen is administered with radioiodine (RAI), the warnings and precautions for RAI apply to this combination regimen. Refer to the RAI prescribing information for a full list of the warnings and precautions for RAI.
ADVERSE REACTIONS
The most common adverse reactions reported in clinical trials were nausea and headache.
USE IN SPECIFIC POPULATIONS
Pregnancy:
- If Thyrogen is administered with radioiodine, the combination regimen is contraindicated in pregnant women.
- Available data with Thyrogen use in pregnant women are insufficient to evaluate for a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes.
Lactation:
- The concomitant use of Thyrogen and radioiodine (RAI) is contraindicated in lactating women. If Thyrogen is administered with RAI for diagnostic use, discontinue breastfeeding after RAI administration because of the potential for serious adverse reactions from RAI in the breastfed infant.
- If Thyrogen is not administered with RAI, the developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Thyrogen and any potential adverse effects on the breastfed child. There are no available data on the presence of thyrotropin alfa in human milk, the effects on the breastfed infant, or the effects on milk production.
Pediatric Use: Safety and effectiveness in pediatric patients have not been established.
Geriatric Use: Results from controlled trials do not indicate a difference in the safety and efficacy of Thyrogen between adult patients less than 65 years and those over 65 years of age.
Renal Impairment: Elimination of Thyrogen is significantly slower in dialysis-dependent end stage renal disease patients, resulting in prolonged elevation of TSH levels.
INDICATIONS AND USAGE
Thyrogen® (thyrotropin alfa) is a thyroid stimulating hormone indicated for:
Adjunctive Diagnostic Tool for Well-Differentiated Thyroid Cancer: Use as an adjunctive diagnostic tool for serum thyroglobulin (Tg) testing with or without radioiodine imaging in the follow-up of patients with well-differentiated thyroid cancer who have previously undergone thyroidectomy.
Limitations of Use:
- Thyrogen-stimulated Tg levels are generally lower than, and do not correlate with Tg levels after thyroid hormone withdrawal.
- Even when Thyrogen-Tg testing is performed in combination with radioiodine imaging, there remains a risk of missing a diagnosis of thyroid cancer or underestimating the extent of the disease.
- Anti-Tg Antibodies may confound the Tg assay and render Tg levels uninterpretable.
Adjunct for Thyroid Remnant Ablation in Well-Differentiated Thyroid Cancer: Use as an adjunctive treatment for radioiodine ablation of thyroid tissue remnants in patients who have undergone a near-total or total thyroidectomy for well-differentiated thyroid cancer and who do not have evidence of distant metastatic thyroid cancer.
Limitations of Use:
- The effect of Thyrogen on thyroid cancer recurrence greater than 5 years post-remnant ablation has not been evaluated.
Click here for full Prescribing Information
.png)