-
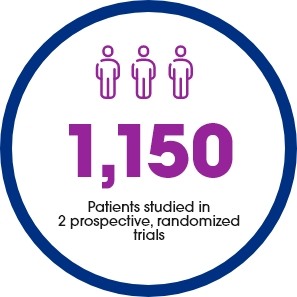
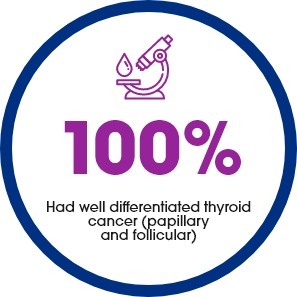
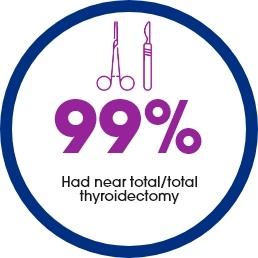
Thyrogen was compared with THW using 2 different doses of radioiodine in patients with well-differentiated thyroid cancer who had undergone thyroidectomy. To date, these are the 2 largest, prospective, multicenter, randomized studies performed in thyroid cancer.1,2
-
In both studies, patients were randomized to 1 of 4 treatment groups: Thyrogen + 30 mCi, Thyrogen + 100 mCi, THW + 30 mCi, THW +100 mCi. There was no difference in the treatment success rates between the 2 doses of radioiodine.
-
Ablation success rates were assessed at approximately 8 months.
The two studies compared the following:
-
Safety and Ablation efficacy between patients prepared with Thyrogen and thyroid hormone withdrawal (THW)
-
Symptoms of acute hypothyroidism before, during, and after Thyrogen injections and thyroid hormone withdrawal (THW).
-
Recurrence rates 5 years after radioactive iodine treatment
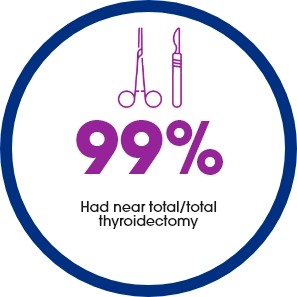
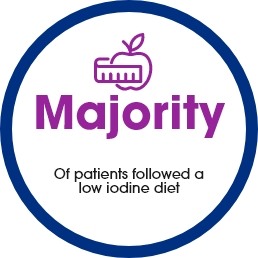
What You Should Know About the Adult Patients in These Studies1,2





Ablation Success at 8 Months: Data from the 2 largest, randomized clinical trials in differentiated thyroid cancer1,2
Successful remnant ablation rates (HiLo Study1): Randomized 438 patients (tumor stages T1-T3, Nx, N0 and N1, M0)

Successful remnant ablation rates (ESTIMABL Study2): randomized 752 low risk patients

In a study with 63 patients, researchers evaluated the quality of life across eight areas using the SF-36 Scale.3
- The Short-Form 36-Item Health Survey (SF-36) is a clinically validated assessment tool commonly used in clinical trials. A higher score indicates a better response.
- The scores were taken at baseline, 2 weeks after randomization, and immediately before RAI ablation for all patients who were randomized into two trial arms: Thyrogen and thyroid hormone withdrawal (THW) plus 100 mCI radioactive iodine.
- The Quality of Life in patients following Thyrogen administration improved in 7of 8 domains between baseline and week 4, whereas the THW group experienced a decrease in 7of 8 QOL measures.
Mean change in SF-36 scores from baseline to week 43
Patients prepared with Thyrogen improved in seven of eight physical and mental domains between baseline and week 4.
The Short-Form 36-Item Health Survey (SF-36) is a clinically validated assessment tool commonly used in clinical trials. A higher score indicates a better response.

In the HiLO and ESTIMABL studies, Thyrogen patients had their cancer return at a similar rate as patients who underwent thyroid hormone withdrawal (THW) after radioactive iodine (RAI) ablation.4,5
Long-term follow-up results from 2 large studies (1150 patients) on thyroid cancer show that Thyrogen had similar results compared with THW for radioactive iodine ablation.
- Cancer recurrence was similar across patients in the Thyrogen and THW groups.1,2
- Overall patients receiving Thyrogen, demonstrated lower deterioration of HRQoL scores compared to those who experienced THW. This is because Thyrogen may help lower the symptoms associated with acute hypothyroidism.
Results of two clinical studies showed that at 5 years recurrence rates after RAI ablation are similar between Thyrogen and thyroid hormone withdrawal (THW)
In low-risk well differentiated thyroid cancer (WDTC) patients, less than 2% had their cancer return at 5 years4
In the ESTIMABL study with 726 patients who received RAI, outcomes were comparable in the different patient groups. Among the patients who had their cancer return, 7 (1.9%) received Thyrogen and 4 (1.1%) received THW.1

In low to intermediate risk well differentiated thyroid cancer patients, cancer recurrence rates were similar between those who received Thyrogen vs THW at 5 years5
In the HiLO study with 438 patients who received RAI, disease recurrence rates were similar among patients in the Thyrogen group vs those in the THW group (2.1% vs. 2.7%).2
Percentage of patients with recurrence at 5 years

Recurrence was similarly low
Thyrogen patients reported better physical and psychological function than those who experienced thyroid hormone withdrawal (THW)
Thyrogen patients had better quality of life compared with THW while undergoing preparation for ablation.
In the HiLo study with 438 patients, quality of life was evaluated at the time of consent, on the day of ablation before radioiodine administration, and 3 months after ablation.
Before ablation, among patients receiving Thyrogen, there were clear benefits as compared with those undergoing THW for physical and psychological functioning.4

Fewer Thyrogen patients reported having difficulty performing their usual activities at home and work
On the day of ablation, patients also completed a questionnaire about thyroid cancer–specific symptoms.
In patients reporting symptoms as either "moderate" or "a lot" fewer Thyrogen patients had difficulty performing usual household activities (13.2% vs 19.2%) or taking care of their children (8.1% vs 14.1%) compared to patients undergoing THW. Among the patients who were employed, fewer patients in the Thyrogen group had difficulty performing usual activities at work compared with the THW group (9.4% vs 22.1%).4
In the same study, out of 438 patients1

Thyrogen was compared with THW using 2 different doses of radioiodine in patients with well-differentiated thyroid cancer who had undergone thyroidectomy. To date, these are the 2 largest, prospective, multicenter, randomized studies performed in thyroid cancer.1,2
-
In both studies, patients were randomized to 1 of 4 treatment groups: Thyrogen + 30 mCi, Thyrogen + 100 mCi, THW + 30 mCi, THW +100 mCi. There was no difference in the treatment success rates between the 2 doses of radioiodine.
-
Ablation success rates were assessed at approximately 8 months.
The two studies compared the following:
-
Safety and Ablation efficacy between patients prepared with Thyrogen and thyroid hormone withdrawal (THW)
-
Symptoms of acute hypothyroidism before, during, and after Thyrogen injections and thyroid hormone withdrawal (THW).
-
Recurrence rates 5 years after radioactive iodine treatment
What You Should Know About the Adult Patients in These Studies1,2





Ablation Success at 8 Months: Data from the 2 largest, randomized clinical trials in differentiated thyroid cancer1,2
Successful remnant ablation rates (HiLo Study1): Randomized 438 patients (tumor stages T1-T3, Nx, N0 and N1, M0)

Successful remnant ablation rates (ESTIMABL Study2): randomized 752 low risk patients

In a study with 63 patients, researchers evaluated the quality of life across eight areas using the SF-36 Scale.3
- The Short-Form 36-Item Health Survey (SF-36) is a clinically validated assessment tool commonly used in clinical trials. A higher score indicates a better response.
- The scores were taken at baseline, 2 weeks after randomization, and immediately before RAI ablation for all patients who were randomized into two trial arms: Thyrogen and thyroid hormone withdrawal (THW) plus 100 mCI radioactive iodine.
- The Quality of Life in patients following Thyrogen administration improved in 7of 8 domains between baseline and week 4, whereas the THW group experienced a decrease in 7of 8 QOL measures.
Mean change in SF-36 scores from baseline to week 43
Patients prepared with Thyrogen improved in seven of eight physical and mental domains between baseline and week 4.
The Short-Form 36-Item Health Survey (SF-36) is a clinically validated assessment tool commonly used in clinical trials. A higher score indicates a better response.

In the HiLO and ESTIMABL studies, Thyrogen patients had their cancer return at a similar rate as patients who underwent thyroid hormone withdrawal (THW) after radioactive iodine (RAI) ablation.4,5
Long-term follow-up results from 2 large studies (1150 patients) on thyroid cancer show that Thyrogen had similar results compared with THW for radioactive iodine ablation.
- Cancer recurrence was similar across patients in the Thyrogen and THW groups.1,2
- Overall patients receiving Thyrogen, demonstrated lower deterioration of HRQoL scores compared to those who experienced THW. This is because Thyrogen may help lower the symptoms associated with acute hypothyroidism.
Results of two clinical studies showed that at 5 years recurrence rates after RAI ablation are similar between Thyrogen and thyroid hormone withdrawal (THW)
In low-risk well differentiated thyroid cancer (WDTC) patients, less than 2% had their cancer return at 5 years4
In the ESTIMABL study with 726 patients who received RAI, outcomes were comparable in the different patient groups. Among the patients who had their cancer return, 7 (1.9%) received Thyrogen and 4 (1.1%) received THW.1

In low to intermediate risk well differentiated thyroid cancer patients, cancer recurrence rates were similar between those who received Thyrogen vs THW at 5 years5
In the HiLO study with 438 patients who received RAI, disease recurrence rates were similar among patients in the Thyrogen group vs those in the THW group (2.1% vs. 2.7%).2
Percentage of patients with recurrence at 5 years

Recurrence was similarly low
Thyrogen patients reported better physical and psychological function than those who experienced thyroid hormone withdrawal (THW)
Thyrogen patients had better quality of life compared with THW while undergoing preparation for ablation.
In the HiLo study with 438 patients, quality of life was evaluated at the time of consent, on the day of ablation before radioiodine administration, and 3 months after ablation.
Before ablation, among patients receiving Thyrogen, there were clear benefits as compared with those undergoing THW for physical and psychological functioning.4

Fewer Thyrogen patients reported having difficulty performing their usual activities at home and work
On the day of ablation, patients also completed a questionnaire about thyroid cancer–specific symptoms.
In patients reporting symptoms as either "moderate" or "a lot" fewer Thyrogen patients had difficulty performing usual household activities (13.2% vs 19.2%) or taking care of their children (8.1% vs 14.1%) compared to patients undergoing THW. Among the patients who were employed, fewer patients in the Thyrogen group had difficulty performing usual activities at work compared with the THW group (9.4% vs 22.1%).4
In the same study, out of 438 patients1

-
-
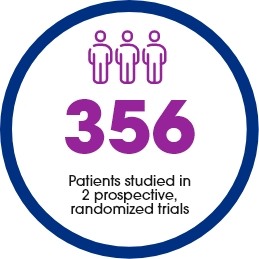
What You Should Know About the Adult Patients in These Diagnostic Studies5,6,7




The two studies compared the following:6,7
- Radioactive iodine whole body scans (WBS) obtained after THYROGEN injections and radioactive iodine whole body scans after thyroid hormone withdrawal (THW).
- Combination of stimulated thyroglobulin (Tg) levels in the blood and WBS obtained after THYROGEN injections and after thyroid hormone withdrawal (THW).
- Symptoms of acute hypothyroidism before, during, and after Thyrogen injections and thyroid hormone withdrawal (THW).
One of the studies with 229 patients, also compared the quality of life between the Thyrogen phase and the THW phase.7
RESULTS comparing patients who received THYROGEN with those prepared with thyroid hormone withdrawal for radioiodine Whole Body Scanning With or Without stimulated thyroglobulin blood testing6,7

Disease detection rates were found to be comparable to the scans after Thyrogen and scans after thyroid hormone withdrawal with or without thyroglobulin testing

A Thyrogen stimulated thyroglobulin detected 100% of patients with metastatic disease vs 79% of patients who received thyroglobulin testing without stimulation
In pooled studies from 6 clinical studies, the most common side effects in patients were nausea, headache, fatigue, vomiting, dizziness and asthenia.6
The Quality of Life in patients following Thyrogen administration in the trial remained similar to their scores before the start of the trial when they were still on thyroid hormone medication.
In one diagnostic study with 229 patients, researchers evaluated quality of life across eight areas using the SF-36 Scale.7
The SF-36 is a 36-item, patient- Best Health reported survey of patient health, consisting of eight scaled scores. The lower the score the more disability. The higher the score the less the disability.
The scores were taken at 3 points in time. At baseline while patients were still on their thyroid hormone medication, after administration of Thyrogen and after TWH on the day of RAI administration.
In this study, patients rated their QOL higher in all eight areas while using Thyrogen to prepare for RAI versus when they underwent THW in preparation for ablation. In fact, in this trial, with 229 patients, the quality of life differences in all eight domains was considered statistically significant.
SF-36 Health Survey Results in the Thyrogen Diagnostic Trial with 229 patients7
Quality of life differences in all eight domains was statistically significant

In two diagnostic studies, researchers evaluated the signs and symptoms of acute hypothyroidism in patients who received 2 injections of Thyrogen compared to by THW.6,7,8 The Billewicz scale was used.
A Billewicz scale is an observer-rated set of clinical findings that has been widely used in assessing hypothyroidism. Higher scores are associated with an increase in signs and symptoms of hypothyroidism.
Billewicz scores were taken at baseline while on thyroid hormone therapy, after administration of Thyrogen and after THW on day of RAI administration
Statistically significant worsening in all measured signs and symptoms were observed during the acute hypothyroid phase for patients undergoing THW
Thyrogen administration was associated with fewer signs and symptoms of hypothyroidism than those associated with thyroid hormone withdrawal as measured by the Billewicz scale.

- Thyrogen is given as a 0.9 mg injection into the muscle of the buttock for two consecutive days
- The most common side effects in patients getting Thyrogen were nausea, headache , fatigue, vomiting, dizziness and asthenia
What You Should Know About the Adult Patients in These Diagnostic Studies5,6,7




The two studies compared the following:6,7
- Radioactive iodine whole body scans (WBS) obtained after THYROGEN injections and radioactive iodine whole body scans after thyroid hormone withdrawal (THW).
- Combination of stimulated thyroglobulin (Tg) levels in the blood and WBS obtained after THYROGEN injections and after thyroid hormone withdrawal (THW).
- Symptoms of acute hypothyroidism before, during, and after Thyrogen injections and thyroid hormone withdrawal (THW).
One of the studies with 229 patients, also compared the quality of life between the Thyrogen phase and the THW phase.7
RESULTS comparing patients who received THYROGEN with those prepared with thyroid hormone withdrawal for radioiodine Whole Body Scanning With or Without stimulated thyroglobulin blood testing6,7

Disease detection rates were found to be comparable to the scans after Thyrogen and scans after thyroid hormone withdrawal with or without thyroglobulin testing

A Thyrogen stimulated thyroglobulin detected 100% of patients with metastatic disease vs 79% of patients who received thyroglobulin testing without stimulation
In pooled studies from 6 clinical studies, the most common side effects in patients were nausea, headache, fatigue, vomiting, dizziness and asthenia.6
The Quality of Life in patients following Thyrogen administration in the trial remained similar to their scores before the start of the trial when they were still on thyroid hormone medication.
In one diagnostic study with 229 patients, researchers evaluated quality of life across eight areas using the SF-36 Scale.7
The SF-36 is a 36-item, patient- Best Health reported survey of patient health, consisting of eight scaled scores. The lower the score the more disability. The higher the score the less the disability.
The scores were taken at 3 points in time. At baseline while patients were still on their thyroid hormone medication, after administration of Thyrogen and after TWH on the day of RAI administration.
In this study, patients rated their QOL higher in all eight areas while using Thyrogen to prepare for RAI versus when they underwent THW in preparation for ablation. In fact, in this trial, with 229 patients, the quality of life differences in all eight domains was considered statistically significant.
SF-36 Health Survey Results in the Thyrogen Diagnostic Trial with 229 patients7
Quality of life differences in all eight domains was statistically significant

In two diagnostic studies, researchers evaluated the signs and symptoms of acute hypothyroidism in patients who received 2 injections of Thyrogen compared to by THW.6,7,8 The Billewicz scale was used.
A Billewicz scale is an observer-rated set of clinical findings that has been widely used in assessing hypothyroidism. Higher scores are associated with an increase in signs and symptoms of hypothyroidism.
Billewicz scores were taken at baseline while on thyroid hormone therapy, after administration of Thyrogen and after THW on day of RAI administration
Statistically significant worsening in all measured signs and symptoms were observed during the acute hypothyroid phase for patients undergoing THW
Thyrogen administration was associated with fewer signs and symptoms of hypothyroidism than those associated with thyroid hormone withdrawal as measured by the Billewicz scale.

- Thyrogen is given as a 0.9 mg injection into the muscle of the buttock for two consecutive days
- The most common side effects in patients getting Thyrogen were nausea, headache , fatigue, vomiting, dizziness and asthenia
Important Safety Information and Indications
Important Safety Information and Indications
IMPORTANT SAFETY INFORMATION
Patients should not use Thyrogen with radioiodine if they have a contraindication to the use of radioiodine. Please consult with your doctor for a list of contraindications for radioiodine.
Thyrogen can cause serious side effects, including:
Thyrogen-Induced Hyperthyroidism:
- There have been reports of events that led to death in patients who have not had surgery to have their thyroid gland removed, and in patients with thyroid cancer cells that have spread to other parts of the body.
- Patients over 65 years old with large amounts of leftover thyroid tissue after surgery, or with a history of heart disease, should discuss with their physicians the risks and benefits of Thyrogen.
- Thyrogen can be administered in the hospital for patients at risk for complications from Thyrogen administration.
Stroke:
- Since Thyrogen was first approved for use, there have been reports of central nervous system problems such as stroke in young women who have a higher chance of having a stroke, and weakness on one side of the body. The relationship between THYROGEN administration and stroke is unknown. Patients should remain hydrated prior to treatment with Thyrogen.
Sudden Rapid Tumor Enlargement:
- Leftover thyroid tissue after surgery and cancer cells that have spread to other parts of the body can quickly grow and become painful after Thyrogen administration. Patients with cancer cells near their windpipe, in their central nervous system, or in their lungs may need treatment with a glucocorticoid (a medication to help prevent an increase in the size of the cancer cells before using Thyrogen.)
Risks Associated with Radioiodine Treatment:
- If THYROGEN is administered with radioiodine (RAI), the serious side effects for RAI apply to this combination regimen. Please consult with your doctor for a list of contraindications for radioiodine.
ADVERSE REACTIONS
In clinical studies, the most common side effects reported were nausea and headache.
USE IN SPECIFIC PATIENT POPULATIONS
Pregnant patients: Notify your healthcare provider immediately in the event of a pregnancy. If THYROGEN is administered with radioiodine, the combination regimen should not be used in pregnant women. Thyrogen should be given to a pregnant woman only if the doctor thinks there is a clear need for it.
Breastfeeding patients: If THYROGEN is administered with radioiodine, the combination regimen should not be used in breastfeeding women. It is not known whether Thyrogen can appear in human milk. Breastfeeding women should discuss the benefits and risks of Thyrogen with their physician.
Children: Safety and effectiveness in young patients (under the age of 18) have not been established.
Elderly: Studies do not show a difference in the safety and effectiveness of Thyrogen between adult patients less than 65 years and those over 65 years of age.
Patients with kidney disease: Thyrogen exits the body much slower in dialysis patients and can lead to longer high TSH levels.
INDICATIONS AND USAGE
Thyrogen (thyrotropin alfa) is used to help identify thyroid disease by testing the blood for a hormone called thyroglobulin in the follow up of patients with a certain type of thyroid cancer known as well differentiated thyroid cancer. It is used with or without a radiology test using a form of iodine.
Limitations of Use:
- The effect of Thyrogen on long term thyroid cancer outcomes has not been determined.
- When Thyrogen is used to help detect thyroid cancer, there is still a chance all or parts of the cancer could be missed.
Thyrogen is also used to help patients prepare for treatment with a form of iodine, called radioiodine, to remove leftover thyroid tissue in patients who have had surgery to take out the entire thyroid gland for patients with well differentiated thyroid cancer who do not have signs of thyroid cancer which has spread to other parts of the body.
Limitations of Use:
- In a study of people being prepared for treatment with a form of iodine after thyroid surgery, results were similar between those who received Thyrogen and those who stopped taking their thyroid hormone for up to 5 years after treatment. Researchers do not know if results would be similar over a longer period of time.
Click here for full Prescribing Information.
References
1) Mallick U, Harmer C, Yap B, et al. Ablation with low-dose radioiodine and thyrotropin alfa in thyroid cancer. N Engl J Med. 2012;366(18):1674-1685.
2) Schlumberger et al. Strategies of Radioiodine Ablation in Patients with Low-Risk Thyroid Cancer. N Engl J Med. 2012 vol. 366 no. 18
3) Pacini et al. Radioiodine Ablation of Thyroid Remnants after Preparation with Recombinant Human Thyrotropin inDifferentiated Thyroid Carcinoma: Results of an International, Randomized, Controlled Study.The Journal of Clinical Endocrinology & Metabolism 91(3):926 –932
4) Schlumberger M, Leboulleux S, Catargi B, et al. Outcome after ablation in patients with low-risk thyroid cancer (ESTIMABL1): 5-year follow-up results of a randomised, phase 3, equivalence trial. Lancet Diabetes Endocrinol. 2018;6(8):618-626.
5) Dehbi HM, Mallick U, Wadsley J, Newbold K, Harmer C, Hackshaw A. Recurrence after low-dose radioiodine ablation and recombinant human thyroid stimulating hormone for differentiated thyroid cancer (HiLo): long-term results of an open-label, non-inferiority randomized controlled trial. Lancet Diabetes Endocrinol. 2019;7(1):44-51.
6) Thyrogen Prescribing Information. Cambridge, MA: Genzyme Corp; March 2020.
7) Haugen BR, Pacini F, Reiners C, et al. A comparison of recombinant human thyrotropin and thyroid hormone withdrawal for the detection of thyroid remnant or cancer. J Clin Endocrinol Metab. 1999;84(11):3877-3885.
8) Paul W. Ladenson, M.D.et al. Comparison of Administration of Recombinant Human Thyrotropin with Withdrawal of Thyroid Hormone for Radioactive Iodine Scanning in Patients with Thyroid Carcinoma; N Engl J Med 1997; 337:888-896
Important Safety Information and Indications
IMPORTANT SAFETY INFORMATION
Patients should not use Thyrogen with radioiodine if they have a contraindication to the use of radioiodine. Please consult with your doctor for a list of contraindications for radioiodine.
Thyrogen can cause serious side effects, including:
Thyrogen-Induced Hyperthyroidism:
- There have been reports of events that led to death in patients who have not had surgery to have their thyroid gland removed, and in patients with thyroid cancer cells that have spread to other parts of the body.
- Patients over 65 years old with large amounts of leftover thyroid tissue after surgery, or with a history of heart disease, should discuss with their physicians the risks and benefits of Thyrogen.
- Thyrogen can be administered in the hospital for patients at risk for complications from Thyrogen administration.
Stroke:
- Since Thyrogen was first approved for use, there have been reports of central nervous system problems such as stroke in young women who have a higher chance of having a stroke, and weakness on one side of the body. The relationship between THYROGEN administration and stroke is unknown. Patients should remain hydrated prior to treatment with Thyrogen.
Sudden Rapid Tumor Enlargement:
- Leftover thyroid tissue after surgery and cancer cells that have spread to other parts of the body can quickly grow and become painful after Thyrogen administration. Patients with cancer cells near their windpipe, in their central nervous system, or in their lungs may need treatment with a glucocorticoid (a medication to help prevent an increase in the size of the cancer cells before using Thyrogen.)
Risks Associated with Radioiodine Treatment:
- If THYROGEN is administered with radioiodine (RAI), the serious side effects for RAI apply to this combination regimen. Please consult with your doctor for a list of contraindications for radioiodine.
ADVERSE REACTIONS
In clinical studies, the most common side effects reported were nausea and headache.
USE IN SPECIFIC PATIENT POPULATIONS
Pregnant patients: Notify your healthcare provider immediately in the event of a pregnancy. If THYROGEN is administered with radioiodine, the combination regimen should not be used in pregnant women. Thyrogen should be given to a pregnant woman only if the doctor thinks there is a clear need for it.
Breastfeeding patients: If THYROGEN is administered with radioiodine, the combination regimen should not be used in breastfeeding women. It is not known whether Thyrogen can appear in human milk. Breastfeeding women should discuss the benefits and risks of Thyrogen with their physician.
Children: Safety and effectiveness in young patients (under the age of 18) have not been established.
Elderly: Studies do not show a difference in the safety and effectiveness of Thyrogen between adult patients less than 65 years and those over 65 years of age.
Patients with kidney disease: Thyrogen exits the body much slower in dialysis patients and can lead to longer high TSH levels.
INDICATIONS AND USAGE
Thyrogen (thyrotropin alfa) is used to help identify thyroid disease by testing the blood for a hormone called thyroglobulin in the follow up of patients with a certain type of thyroid cancer known as well differentiated thyroid cancer. It is used with or without a radiology test using a form of iodine.
Limitations of Use:
- The effect of Thyrogen on long term thyroid cancer outcomes has not been determined.
- When Thyrogen is used to help detect thyroid cancer, there is still a chance all or parts of the cancer could be missed.
Thyrogen is also used to help patients prepare for treatment with a form of iodine, called radioiodine, to remove leftover thyroid tissue in patients who have had surgery to take out the entire thyroid gland for patients with well differentiated thyroid cancer who do not have signs of thyroid cancer which has spread to other parts of the body.
Limitations of Use:
- In a study of people being prepared for treatment with a form of iodine after thyroid surgery, results were similar between those who received Thyrogen and those who stopped taking their thyroid hormone for up to 5 years after treatment. Researchers do not know if results would be similar over a longer period of time.
Click here for full Prescribing Information.
References
1) Mallick U, Harmer C, Yap B, et al. Ablation with low-dose radioiodine and thyrotropin alfa in thyroid cancer. N Engl J Med. 2012;366(18):1674-1685.
2) Schlumberger et al. Strategies of Radioiodine Ablation in Patients with Low-Risk Thyroid Cancer. N Engl J Med. 2012 vol. 366 no. 18
3) Pacini et al. Radioiodine Ablation of Thyroid Remnants after Preparation with Recombinant Human Thyrotropin inDifferentiated Thyroid Carcinoma: Results of an International, Randomized, Controlled Study.The Journal of Clinical Endocrinology & Metabolism 91(3):926 –932
4) Schlumberger M, Leboulleux S, Catargi B, et al. Outcome after ablation in patients with low-risk thyroid cancer (ESTIMABL1): 5-year follow-up results of a randomised, phase 3, equivalence trial. Lancet Diabetes Endocrinol. 2018;6(8):618-626.
5) Dehbi HM, Mallick U, Wadsley J, Newbold K, Harmer C, Hackshaw A. Recurrence after low-dose radioiodine ablation and recombinant human thyroid stimulating hormone for differentiated thyroid cancer (HiLo): long-term results of an open-label, non-inferiority randomized controlled trial. Lancet Diabetes Endocrinol. 2019;7(1):44-51.
6) Thyrogen Prescribing Information. Cambridge, MA: Genzyme Corp; March 2020.
7) Haugen BR, Pacini F, Reiners C, et al. A comparison of recombinant human thyrotropin and thyroid hormone withdrawal for the detection of thyroid remnant or cancer. J Clin Endocrinol Metab. 1999;84(11):3877-3885.
8) Paul W. Ladenson, M.D.et al. Comparison of Administration of Recombinant Human Thyrotropin with Withdrawal of Thyroid Hormone for Radioactive Iodine Scanning in Patients with Thyroid Carcinoma; N Engl J Med 1997; 337:888-896
.png)